We all know stroke is a possibility, but until you live it—until you are scrambling in the middle of the night—you really have no clue what to expect.
That feeling of guilt, of wishing you were there, is heavy, and it’s valid. This moment of crisis demands a different kind of preparation.
This post offers a detailed, general guide for caregivers on what happens right after a loved one has a stroke, focusing on the emergency room and hospital phases. No two strokes are the same, but knowing the process can help you feel grounded when everything else is chaos.
1. The Immediate Crisis: Recognizing the Signs
A stroke occurs when a blood supply to the brain is blocked by a clot (Ischemic, 87% of cases) or a burst blood vessel (Hemorrhagic). Every minute matters, as 32,000 brain cells die every second during an ischemic stroke.
While you may not have witnessed the onset, knowing the signs is crucial for immediate and future episodes.
Key Warning Signs to Watch For
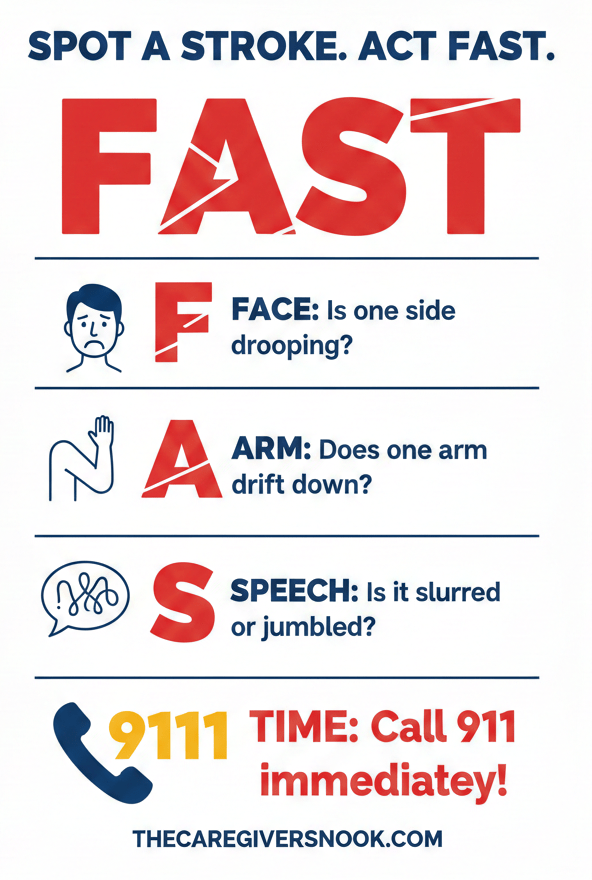
Remember, these symptoms appear suddenly:
- Sudden Numbness/Weakness: Especially on one side of the face, arm, or leg.
- Confusion: Difficulty understanding or speaking.
- Vision Problems: Sudden loss or change in one or both eyes.
- Trouble Walking: Sudden dizziness, loss of balance, or feeling unsteady.
- Severe Headache: An intense headache with absolutely no known cause.
It’s natural to carry guilt about what you didn’t see. Your focus must now shift entirely to managing the present and the future.
2. Arrival at the Emergency Department: What to Expect

Upon arrival at the ED, the medical team is in a race against time.
Initial Assessment and Stabilization
The first priority is assessing the immediate danger and stabilizing the patient. This involves:
- Vitals Check: Monitoring heart rate, blood pressure, temperature, and oxygen.
- IV Access: Placing an IV line for immediate medication.
- Glucose Check: Performing a blood draw, as low blood sugar can mimic stroke symptoms.
- Neurological Exam: Checking the patient’s ability to move, speak, and feel.
- NIHSS Scale: Using the National Institutes of Health Stroke Scale to measure the severity of the neurological damage.
Diagnosis and Treatment (The Crucial Window)
The next steps are critical, often happening within the first hour:
- CT Scan: A CT scan is rushed to identify the stroke type: Ischemic (clot) or Hemorrhagic (bleeding).
- Clot-Busting Treatment (Ischemic): If the stroke is ischemic and the patient is eligible, they may be given tPA (thrombolytics), a clot-busting medication.
- Surgical Intervention (Hemorrhagic): For bleeding strokes, surgery may be necessary to repair the damaged vessel.
- Thrombectomy: In some cases, a procedure to surgically remove the clot may be performed.
Why the ICU?
Many severe stroke victims are taken to the Intensive Care Unit (ICU) for continuous, specialized monitoring. This happens when the stroke causes:
- Breathing or Airway Problems: Requiring intubation and mechanical ventilation.
- Decreased Consciousness: Requiring high-level support.
- Complications: Such as severe brain swelling or circulatory issues.
3. The Path to Recovery: Rehabilitation Options
Recovery and rehabilitation are a marathon, not a sprint. Rehabilitation often starts as soon as the patient is medically stable—sometimes within 24 hours.
Post-Acute Care Options
The discharge from the hospital or ICU often leads to one of several long-term care settings, depending on the severity of the stroke and the patient’s needs:
- Inpatient Rehabilitation Facilities (IRFs): Recommended for medically stable survivors who can tolerate intensive daily therapy (three or more hours per day).
- Skilled Nursing Facilities (SNFs): Offers skilled nursing care, therapy, and rehabilitation for patients who need ongoing care but cannot handle the intensity of an IRF.
- Long-Term Acute Care (LTAC): For patients with complex and serious medical conditions requiring intensive, physician-led care (like respiratory support).
Discharging Home vs. Nursing Home
The goal is always to return home, but the high level of care required means some survivors may need placement in a long-term Nursing Home.
Key factors for a discharge to home include:
- The survivor’s ability to manage daily tasks (eating, dressing, mobility).
- The availability of a strong support system (the caregiver—you).
- The safety and accessibility of the home environment.
Discharge planning involves setting up follow-up services like Outpatient Therapy or Home Health Care (nursing, physical, and occupational therapy delivered in the home).
If you are weighing your options, we offer a comprehensive comparison in our guide: The Ultimate Guide to Choosing Between In-Home Care and Assisted Living .
Before making a final decision, it’s essential to explore all your options, including a deep dive into the differences between in-home care and assisted living , which we cover in detail elsewhere on our site.
Strokes Suck, But You’re Not Alone
The statistics are grim: stroke is the leading cause of serious long-term disability, and two-thirds of survivors are disabled. You are facing a lifetime of dedication, and it is natural to feel overwhelmed.
I encourage you to use this information to speak confidently with doctors and make informed decisions. You are doing an incredible job learning as you go. Share this with anyone who might benefit—the knowledge itself is a powerful tool in this fight.
You are a strong caregiver, and you are not alone.


